 In practice life a number of questions arise relating to all supplemental suggestions and vitamin D is no different.
In practice life a number of questions arise relating to all supplemental suggestions and vitamin D is no different.
• What do I need to be healthy?
• How do I know what my levels are now?
• How do I raise my levels if I need to?
• What foods, supplements or lifestyle changes do I need to do?
What do I actually need to be healthy
Chief Medical Officer for England Professor Dame Sally Davies said:
“A significant proportion of people in the UK probably have inadequate levels of vitamin D in their blood.”
In the UK the government agency: the Department of Health defines you as being deficient in vitamin when: blood serum level of Vitamin D [ 25(OH)D) ] are less than 25 nmol/L (nanomols per Litre).[1]
For US conversion
25 nmol/L = 10 ng/mL (nanograms per millilitre)
In the USA the Institute of Medicine ( IOM ) set the equivalent level at 50 nmol/L in their report issued in November 2010.[2]
These levels are regarded as highly conservative by many of the world’s leading experts in Vitamin D research. However, the uncertainty suggested by the IOM report continues to niggle away at many clinicians as another more recent paper suggests.[3]
The decision infuriated many scientists—some of whom had published a correlation between high blood levels of vitamin D and reductions in the rates of many diseases.
Nutrients act through multiple mechanisms, and low intakes might be expected to lead to disorders quite distinct from the disease originally connected with the nutrient. Vitamin D is a good case in point. Total body inputs closer to those that must have prevailed during hominid evolution are associated with reduced risk of disorders as varied as Type I diabetes,: colorectal cancer, diabetes, asthma, influenza, multiple sclerosis, and an array of other ailments.[4]
Researchers have regularly demonstrated many ways the vitamin might bring about benefits:
The hormone derived from vitamin D, called 1,25-dihydroxyvitamin D3, or calcitriol, is responsible for turning on or off hundreds of genes in the body, thereby participating in processes ranging from cell proliferation to immune system regulation.
But the IOM panel concluded that without large-scale prevention trials confirming the ultimate result of high levels of vitamin D, it could not say for certain whether insufficiency contributes to cancer or any other non-skeletal disease.
Many of the leading scientists involved in these correlational studies continue to argue that their studies provide enough evidence to safely recommend that people maintain a higher concentration of vitamin D in their blood. They point out that difficult, expensive, and often inconclusive prevention trials, particularly those for relatively rare or unpredictable diseases, are a waste of time.
“The success of the RCT [randomised controlled trial] in evaluating medical treatments has, perhaps, blinded nutritionists, regulators, and editors to the fact that it is a method ill-suited for the evaluation of nutrient effects,”
..so Robert Heaney, an endocrinologist at Creighton University School of Medicine stated in a 2008 commentary published in The Journal of Nutrition.[5]
Experts Vary
At the more conservative end of the scale published reports support the definition of sufficiency, serum levels of 25-hydroxyvitamin D [25(OH)D] greater than 30 ng/mL (75 nmol/L). To achieve this, most people need vitamin D supplementation ranging from 600 to 2000 IU/day; consumption up to of 5000 international units (IU) per day of vitamin D is reported as safe.
Although light-skinned individuals need 1000 IU/day of vitamin D, elderly and dark-skinned individuals are likely to need approximately 2000 IU/day to maintain serum 25(OH)D levels greater than 30 ng/mL.
Other vulnerable patients, such as the obese, those who have undergone bariatric surgery, and those with gastrointestinal malabsorption syndromes, may require higher doses of vitamin D to maintain normal serum levels and be healthy.
Professor Robert Heaney, says that Vitamin D “enables the body to absorb calcium” and that the level should be set at 100 nmol/L
Professor Bruce Hollis, who is a world expert in Vitamin D for pregnant women and their babies, says that the baby takes nutrients from the mother and that pregnant women should have 125 nmol/L
Recent evidence reveals beneficial effects of vitamin D at serum levels around 50 ng/mL (125 nmol/L)[6],[7],[8] or higher – effects not seen at levels below 40 ng/mL (120 nmol/L), indicating a need for upward revision of the deficiency reference threshold.
Based on the data, it is reasonable to assume that, should the threshold for vitamin D deficiency be raised to a level of 50 ng/mL (125 nmol/L), the percentage of the population determined to be deficient would most-likely be closer to 90% or greater
Another group of approximately 40 experts in vitamin D have requested through their call to action that blood levels should aim to be between 100-150 nmol/L.[9]
So, you choose your expert and you set your own levels
How do I know what my levels are now?
The only reliable way to know is to have a blood test for 25-hydroxyVitaminD or 25(OH)D
The options are:
- Ask your GP/Doctor for a test.
- Have the test done privately
Due to the big numbers of people asking their GP for a test some are only offering one a year – not much use if you want to know if your intervention strategy has been successful!
If your GP provides a test – keep the results or a copy of them in a place you can find them again to check any changes against.
If you want to have the test done privately there is an NHS hospital in Birmingham that offers the test direct to the public/practitioners.
Until Mar 31 the test costs £20 making this a very reasonable investigation option. It will rise to £25 from April 1. Find out more here: www.vitamindtest.org.uk or phone +44 (0)121 507 4278
Other labs offer the test following a referral.
www.biolab.co.uk and www.tdlpathology.com
What foods, supplements or lifestyle changes do I need to do ?
The results you get back from the lab will likely vary a great deal from the optimal range and may be spread from lows of 10 nmol/L to highs of 200 nmol/L. These may also include a lab opinion on the relevance compared to ideal ranges.
Based on the readings already discussed of achieving at least 75nmol/L it is likely you will need to supplement.
To assist with planning doses, consider that consuming 25 micrograms ( = 1,000 IU ) of Vitamin D3 per day for 3 months will raise your level by 25 nmol/L. This guide works well when you are below 100 nmol/L, but you will need increasingly large amounts above 100 nmol/L as the body self-regulates. This will also vary depending on your body mass, colour and age.
Rule of thumb:
Per 1000iu/day:
A 50nmol/L or 10ng/ml rise starting at baseline of: 10ng/ml,
Only 20 nmol/L or 8ng/ml rise starting at baseline of: 30ng/ml,
Only 12.5nmol/L or 5ng/ml rise starting at baseline of: 125nmol/L or 50ng/ml.
Here are some examples:
| Result (nmol/L) | 25 | 50 | 25 | 50 |
| Target (nmol/L) | 75 | 75 | 100 | 150 |
| Requirement (IU / day) | 2,000 | 1,000 | 3,000 | 4,000 |
| (Micrograms per day) | 50 | 25 | 75 | 100 |
Vitamin D can be taken once a week, since the half-life of Vitamin D in the body is 14-30 days. Multiply the daily amount by 7 and take approximately that amount once a week.
Cautions
A small number of people have a genetic problem with Vitamin D, such as sufferers from Sarcoidosis (too sensitive) or Coelic disease (not sensitive enough).
During pregnancy there remains some questions, with the UK government recommending intake of 10mcg (μg) per day or 400iu. Obviously this is a lot lower than many researchers recommend, and considering the impact that vitamin D has on the foetal health it is recommended a vitamin D test is undertaken and supplementation recommended to meet the needs of the individual.[10]
What foods, supplements or lifestyle changes do I need to do?
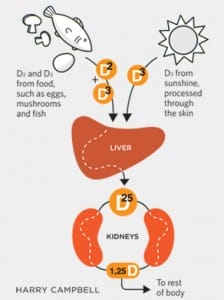
Vitamin D is a fat-soluble vitamin that is naturally present in very few foods, added to others, and available as a dietary supplement. It is also produced endogenously when ultraviolet rays from sunlight strike the skin and trigger vitamin D synthesis. Vitamin D obtained from sun exposure, food, and supplements is biologically inert and must undergo two hydroxylations in the body for activation. The first occurs in the liver and converts vitamin D to 25-hydroxyvitamin D [25(OH)D], also known as calcidiol. The second occurs primarily in the kidney and forms the physiologically active 1,25-dihydroxyvitamin D [1,25(OH)2D], also known as calcitriol
Very few foods in nature contain vitamin D. The flesh of fatty fish (such as salmon, tuna, and mackerel) and fish liver oils are among the best sources [11]. Small amounts of vitamin D are found in beef liver, cheese, and egg yolks. Vitamin D in these foods is primarily in the form of vitamin D3 and its metabolite 25(OH)D3.[12] Some mushrooms provide vitamin D2 in variable amounts.[13] Mushrooms with enhanced levels of vitamin D2 from being exposed to ultraviolet light under controlled conditions are also available.
The other alternative is to expose your body, without sunscreen, to direct sunlight – but only when your shadow is shorter than your height. This is only possible in the UK between April and September between about 10:00am and 4:00pm. Do not burn your body and cover up if your body begins to become pink. A white skinned person will receive 20,000 IU within 15 minutes, but an Asian person might need 30-60 minutes and an African person might need 1-2 hours in the direct sun.
Further information may be found at: www.rufusgreenbaum.com whose blog provided materials, data and inspiration for this piece.
References
[1] Data from years 1 & 2 of the National Diet and Nutrition Survey (NDNS) rolling programme. Low status is defined by the Department of Health as a plasma concentration of 25-hydroxyvitamin D (25(OH)D, the main circulating form of the vitamin) of below 25nmol/l (equal to 10 ng/ml). View Letter
[2] Dietary Reference Intakes for Calcium and Vitamin D IOM Report Nov 2010. View Report
[3] M. Chung et al., “Vitamin D with or without calcium supplementation for prevention of cancer and fractures: An updated meta-analysis for the US Preventive Services Task Force,” Ann Intern Med, 155:827-38, 2011 View Abstract
[4] . Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006;81:353–73. View Abstract
[5] R.P. Heaney, “Nutrients, endpoints, and the problem of proof,” J Nutr, 138:1591-95, 2008. View Full Paper
[6] Davis, W. Rockway, S. Kwasny, M. Effect of a combined therapeutic approach of intensive lipid management, omega-3 fatty acid supplementation, and increased serum 25 (OH) vitamin D on coronary calcium scores in asymptomatic adults. Am J Ther. 2009 Jul-Aug; 16 (4): 326-32. View Abstract
[7] Seki, T. Yamamoto, M. Ohwada, R. Takano, K. Kure, M. Sekine, H. Katsura, Y. Sato, K. Successful treatment of postsurgical hypoparathyroidism by intramuscular injection of vitamin D3 in a patient associated with malabsorption syndrome due to multiple abdominal surgeries. J Bone Miner Metab. 2010 Mar; 28 (2): 227-32. View Abstract
[8] Garland, C. F. Gorham, E. D. Mohr, S. B. Garland, F. C. Vitamin D for cancer prevention: global perspective. Ann Epidemiol. 2009 Jul; 19 (7): 468-83. View Abstract
[9] http://www.grassrootshealth.net/
[10] De-Regil LM, Palacios C, Ansary A, Kulier R, Peña-Rosas JP. Vitamin D supplementation for women during pregnancy. Cochrane Database Syst Rev. 2012 Feb. View Abstract
[11] Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: National Academy Press, 2010.
[12] Ovesen L, Brot C, Jakobsen J. Food contents and biological activity of 25-hydroxyvitamin D: a vitamin D metabolite to be reckoned with? Ann Nutr Metab 2003;47:107-13. View Abstract
[13] Mattila PH, Piironen VI, Uusi-Rauva EJ, Koivistoinen PE. Vitamin D contents in edible mushrooms. J Agric Food Chem 1994;42:2449-53.






1 Comment. Leave new
Very informative article. Must read by everyone.