 At present no chronic disease has a greater drag on global function than mental illness.[1] A remarkable 40% of the European population is affected in any given year with depressive symptoms, and these numbers are rising.
At present no chronic disease has a greater drag on global function than mental illness.[1] A remarkable 40% of the European population is affected in any given year with depressive symptoms, and these numbers are rising.
Core symptoms include depressed mood, anhedonia (reduced ability to experience pleasure from natural rewards), irritability, difficulties in concentrating, and abnormalities in appetite and sleep (‘neurovegetative symptoms’). In addition to mortality associated with suicide, depressed patients are more likely to develop coronary artery disease and type 2 diabetes. Depression also complicates the prognosis of a host of other chronic medical conditions. The chronic, festering nature of depression contributes substantially to the global burden of disease and disability.
Pharmaceutical manufacturers are currently withdrawing from this field of research, in part because of the complexity of the subject and lack of funding, and in part because of the relative lack of success in drug development for the effective and safe treatment of mental illness. There is evidence that anti-depressants work in severe depression but not mild depression.[2]
There is in the drug world, a degree of hope that the latest genetic technologies will help to identify effective treatment targets, and offer alternatives to the monoamines that have dominated psychiatric medications for half a century but as yet this has not translated into clinical use.
Nutritional therapy may not represent a stand-alone intervention for mental health, but to ignore its relevance in improving outcomes and overall health in the research drive to identify molecular ‘silver bullets’ will simply repeat the manifestly derisory clinical developments in the last few years.
There exists a well-established management of mental health through the judicious utilisation of ‘talking therapies’ including cognitive behavioural therapy (CBT) and many others.[3] In managing people with complex mental health issues, no single therapy has been able to establish completeness of outcomes. Integrating evidence based nutritional recommendations has a low risk to benefit ratio and will be an appealing proposal to those clinicians that recognise the need for integrative care.
People with severe mental health issue need to under the direct care of their medical doctor and support teams, communicating this to anyone seeking the use of food or supplements as their only strategy is very important and represents a genuine red flag for all practitioners.
Lifestyle Medicine for Mental Health Resolution and Prevention
Exercise and dietary selection, recognised as a valid medicine since man first began to record methods of improving health have an historical and developing role in prevention and treatment.[4]

A healthy Mediterranean-style diet for example is thought to be protective as is regular exercise — so combining a regular dance class with a big Greek salad and a glass of red wine may make very attractive therapy.[5],[6]
Over the past decade, multiple epidemiological studies have shown that exercise, intellectual activity, social relationships and a healthy diet all lead to a lower risk of mental health problems including dementia and depression. Such findings are generally interpreted with caution by mainstream science, however, as many researchers remain sceptical about the benefits, and because withdrawing from social relationships and other activities can be an early symptom of dementia, not just a risk factor for it.
In terms of depression there are significant changes in researchers’ focus in the last 5-10 years as inflammation induced by lifestyle choices, in particular diet appear to be causally related to depressive behaviour.[7]
Mental Health and Genetics
Depression is so common that it seems the possibility of depression must be “hard-wired” into our brains. This has led biologists to propose several theories to account for how depression, or behaviours linked to it, can somehow offer an evolutionary advantage. For several years, researchers have seen links between depression and inflammation, or over-activation of the immune system. People with depression tend to present with higher levels of inflammation, even if they’re not fighting an infection.
Yet major depression is so detrimental to survival and reproduction that it is hard to understand why allelic variants that promote the disorder have not been culled from the human genome, why in fact, far from being culled, genes that promote depression are so common and numerous and appear to have actually increased in prevalence during recent human evolution.[8] This gene conferred relationship, and the connections between our immune system and mental health are discussed in a recent publication in Molecular Psychiatry.[9]
“The basic idea is that depression and the genes that promote it were very adaptive for helping people—especially young children—not die of infection in the ancestral environment, even if those same behaviours are not helpful in our relationships with other people,”
Psychosocial stress and its effect on mental health may be especially relevant in this regard. Stress is well recognised as a universal and powerful risk for the development of depression both during development and adulthood.[10]
Given this, it is not surprising that, to quote Firdaus Dhabhar,
“Stress perception by the brain may serve as an early warning signal to activate the immune system in preparation for a markedly increased likelihood of subsequent infection”.[11]
So many risks for depression, including obesity, sedentary lifestyle, dietary factors, diminished sleep and smoking, are at least partially non-social in nature but are all associated with increased inflammation suggesting that they may be depressogenic because they tap into pathways that initially evolved to fight infection and to encourage isolated behaviour, which diminished exposure risks and perhaps separated fighting members of the social group.[12],[13]
Dietary strategies clearly influence inflammation, as documented through both prospective observational studies as well as randomised controlled feeding trials in which participants agree to eat only the food provided to them.[14] Indeed, mechanistic studies have shown how various dietary components can modulate sympathetic activity, oxidative stress, transcription factor nuclear factor kappa B (NF-κB) activation, and proinflammatory cytokine production, thus modifying health risks and contributing to reduced risk of mental health problems.[15],[16]
So: Which Foods Are Best for the Brain?
Diet is inextricably and unquestionably linked to conditions such as heart disease, obesity, and diabetes as well as many other chronic illnesses. However, what we consume also seems to have significant implications for the brain: Unhealthy diets may increase risk for psychiatric and neurologic conditions, such as depression and dementia, whereas healthy diets may be protective.
This in turn opens up discussions around food selection, not as an adjunctive therapy to simply aid in recovery, but also as a preventative strategy. The ever increasing burden in terms of social dysfunction and medical cost driven by declining mental health should encourage a greater awareness of how foods, food groups and eating patterns may beneficially reduce this cost burden in our society.
Heading South, Or At Least Acting Greek May Actually Help.
Back in 2009 the journal Archives of General Psychiatry confirmed in a paper that people who followed a dietary lifestyle consistent with the Mediterranean diet benefitted from a number of disease risk reductions including mental health.
After studying more than 10,000 initially healthy Spaniards their results show that those who followed the Mediterranean dietary pattern (MDP) — rich in vegetables, fruits, nuts, whole grains, and fish — were 30% less likely to develop depression during the next 4 years than those who ate more meat, meat products, or whole-fat dairy.[17] In addition, a long favourite in salad dressing – olive oil, shows an intake related reduction in risk of ischaemic stroke.[18] Olive oil and exercise can now add reduction in risk for the development of cognitive decline and Alzheimer’s to their list of related benefits.
We already know that the much promoted ‘poly pill’ advocated as a pharmaceutical solution to lifestyle driven illness had its purported benefits knocked back by the ‘poly meal’, that recommended the Mediterranean diet as its mainstay.[19] This style of eating when accompanied by regular exercise extends its related benefits to mild cognitive impairment and the ever threatening degenerative illness called Alzheimers.[20],[21]
Fat: Which Type Helps?
Our brains are made largely of fat and water, but not just any old fat; it requires special types of fat known as essential fatty acids. As you read this, fats are being incorporated into your brain.
The delicate fatty acid membranes that surround human cells and permit the proteins bound within them to function within the ‘fluid mosaic model’ described by Singer and Nicholson back in 1972 are vulnerable to damage.[22] Recent work suggests that a special fatty acid mix called a glycophospholipid may confer unique oxidative inhibition, repair existing membrane damage and increase ATP production leading to inhibition or prevention of mental ill health.[23],[24]
It has now been proven in human clinical trials that glycophospholipids will restore lost membrane vitality. In an elderly population, individuals consuming six tablets (4000mg) of glycophospholipids per day restored their membrane health to levels normal for young healthy adults in just two months.[25] The implication being that in mental ill health in which ATP production is a feature, restoration by additional glycophospholipid supplementation may produce a clinical benefit greater than that achieved by dietary inclusion of EFA’s alone.
Other Mediterranean studies, these ones from Spain[26],[27] reported that consumption of both polyunsaturated fatty acids (found in nuts, seeds, fish, and leafy green vegetables) and monounsaturated fatty acids (found in olive oil, avocados, and nuts) decreases the risk for depression over time.
By contrast, there were clear dose-response relationships between dietary intake of trans fats, fast foods and depression risk. Trans fats are found extensively in processed foods, including some confectionary. Whilst childhood depression is rising, the incidence of attention deficit disorder is already well recognised and not surprisingly a link between polyunsaturated fatty acid deficiencies is linked to hyperactivity and attention deficit disorders in children.[28]
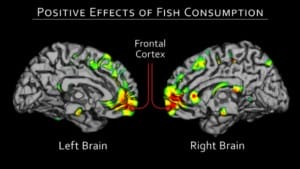
Oily Fish May Prevent Psychosis!
Our early ancestors experienced relatively rapid brain development and intellectual superiority thanks to their abundant source of omega three rich foods harvested from the oceans around the southern coast of Africa.[29] Thanks to their high levels of polyunsaturated fatty acids, namely omega-3 fatty acids, fish it seems can help fend off numerous diseases of the brain.
In 2010, a study using 33,000 women as its reference base found a correlation between fatty acids and vitamin D and a reduced incidence of psychotic like symptoms.[30] A follow up study also found that at risk individuals had a greater chance of avoiding a psychotic episode when consuming fish oils.[31]
It is the nature of long term nutritional studies that data often appears conflicting. Nutrients act through multiple mechanisms, and low intakes might be expected to lead to disorders quite distinct from the disease originally connected with the nutrient.
“The success of the RCT [randomised controlled trial] in evaluating medical treatments has, perhaps, blinded nutritionists, regulators, and editors to the fact that it is a method ill-suited for the evaluation of nutrient effects.” [32]
The long history of food related benefits extends beyond the one pathway one outcome strategy favoured by the pharmaceutical model. Triage theory related to long term modest nutrient deficiencies as proposed by Prof Ames and colleagues proposes a strategic sacrifice of nutrients to ATP promotion that creates deficiency diseases of nutrient latency such as mental ill health.[33]
Newer research pretty consistently shows that the omega-3 fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) are beneficial in both depression and postpartum depression, respectively, and other studies suggest that omega-3 deficiency may be a compounding risk factor for suicide.[34]
In terms of food selection; oily, cold-water fish, such as salmon, herring, and mackerel, have the highest omega-3 levels.
Nutrient Packed Berries Carry An Oxidative Punch.

Berries are generally small nutrient dense fruits that use complex chemical combinations to protect their inner tissues from oxidative stress. These protective agents include polyphenols, namely anthocyanins. Not only are they tasty and nourishing they also hold some remarkable recuperative potential.
Back in 2010 a study using rats – admittedly not humans – found that these tightly bundled chemicals found in berries and other darkly pigmented fruits and vegetables may slow cognitive decline through antioxidant and anti-inflammatory properties. Natural polyphenols in berries and other fruits, vegetables, and nuts are now known to enhance brain health via their antioxidant and anti-inflammatory properties. Many publications using animal models report beneficial effects of berries and walnuts on memory, motor skills, and other behaviour.[35],[36]
An exciting in vitro study demonstrated age-related amyloid plaque deposition reversal and additional neuroprotection in the animals studied, and whilst the doses used are high, this outcome suggests an ancient conserved protective mechanism favoured by food selection.[37] This can be exploited in humans through suitable inclusion of these fruits, especially blueberries, in our daily diet.[38],[39] The researchers also detected a statistical trend towards fewer signs of depression, and lower blood sugar (glucose) levels, among the test group. Berries are attracting increasing interest as their transfer to human application is easy and surprisingly promising.[40]
Wholly Cow! What’s Good For Your Brain Is Good For The Planet, Too!
Already confirmed back in 2010, is that a diet rich in fruits, vegetables, whole grains, high quality meat and fish results in a remarkable 30% reduction in depressive behaviours and anxiety disorders compared to a typical western diet. Typical western diets are high in processed meats, fats and sugars.[41] Yet, very few professionals working with mental illness regard food selection as little more than to provide fuel.
A more recent paper in the journal Archives of Internal Medicine has reawakened the medical and wider community to the risks linked to consumption of processed meats and mortality. This is the first large-scale prospective longitudinal study showing that consumption of both processed and unprocessed red meat is associated with an increased risk of premature mortality from all causes as well as from cardiovascular disease and cancer, all linked to aberrant inflammation and associated inflammation driven depression.[42]
Current farming practices are in part to blame for this increase in red meat related mortality, they have and are changing, driven by the global growth in the human population. Food producers are facing increasing demands on food production and quality suffers. Intensive farming practices increase saturated fat and decrease very important good fatty acids in the meat…pasture-raised animals have a much healthier fatty acid profile.[43]
Booze – If I Must, But Just A Little…
To imbibe or abstain – a long discussed balance that does not always hinge on mental health outcomes! Much to the joy of those that enjoy a glass or two, low to moderate* alcohol consumption has been associated with numerous potential physiologic benefits, including improved cholesterol profiles, beneficial effects on platelet and clotting function, and improved insulin sensitivity.[44]
There is evidence from meta-analysis that moderate intake is linked to a reduction of Alzheimer’s risk[45] and wine has been demonstrated via its polyphenolic compounds to increase cerebro vascular blood flow potentially aiding cognition and mood.[46]
However, the health costs of alcohol consumption beyond low to moderate intake can quickly outweigh benefits to the brain, as heavy and long-term alcohol use can lead to alcohol abuse and dependence, impair memory function, contribute to neurodegenerative disease, and hinder psychosocial functioning.
* In the UK, the recommendation is no more than two to three units of alcohol a day for women and three to four units for men, with at least two or three alcohol-free days each week.
What’s a unit?
One unit of alcohol is 10 ml (1 cl) by volume, or 8 g by weight, of pure alcohol. For example:
- One unit of alcohol is about equal to:
- half a pint of ordinary strength beer, lager, or cider (3-4% alcohol by volume), or
- a small pub measure (25 ml) of spirits (40% alcohol by volume), or
- a standard pub measure (50 ml) of fortified wine such as sherry or port (20% alcohol by volume)
Caffeine and CNS Impact

No other psychoactive drug is consumed more enthusiastically than caffeine infused beverages, and whilst there are many contradictory reports on its potential risks and benefits there is a steady trend of support for certain mental health risks being reduced.
Another meta-analysis (not my favourite type of research) suggested that consumption of between 1 and six(!) cups reduce the risk for stroke by 17%. This outcome suggests a conflicting or at least a negating role between the antioxidant benefits in coffee that diminishes oxidative damage of LDL cholesterol whilst also increasing a primary risk factor for stroke – blood pressure.[47] Further support for the daily infusion may be found in a paper that suggests insulin sensitivity is increased and inflammatory markers reduced by ingesting caffeine.[48]
So does this have any effect on depressive behaviour? There does appear to be a related dose dependent benefit, with women who drink 2-3 cups per day demonstrating a 15% decreased risk for depression compared to their peers who drank just 1 cup daily. Increasing the intake to 4 cups per day saw the risks decrease by 20%.
So what are the mechanisms that may account for this? Serotonin and dopamine responses are improved in the short term response and antioxidant and anti-inflammatory benefits may diminish the cytokine burden linked to depressive illness already discussed.[49]
Habitual caffeine consumers who abstain from caffeine experience withdrawal symptoms such as headache, fatigue, difficulty concentrating, mood disturbances, and flu-like symptoms.[50] The caffeine withdrawal syndrome has been documented across many experimental studies suggesting its ingestion is not without risks of dependency and increased tolerance resulting in increased ingestion. The withdrawal syndrome has an onset at 12-24 h, peak at 20-48 h, and duration of about 1 week.
Although more research is clearly needed, coffee, when consumed without added cream or sugar, is a calorie-free beverage that may confer some mental health benefits, especially when used in individuals who do not have adverse subjective effects due to its stimulating effects, and when coffee is substituted for less healthy, unnatural, and/or high-calorie beverages, such as colas and other sugary and artificially sweetened sodas and soft drinks.[51]
Cacao And Its Sweet Benefits
Dark chocolate (>70%) has been described as mood food, and whilst a great deal of anecdotal evidence exists that chocolate affects mood, there is still some debate as to whether it reduces depressive behaviour or is consumed as part of depressive behaviour.[52],[53]
Chocolate’s mood state effects are purported to be due to its many psychoactive ingredients, including several biogenic stimulant amines, two analogues of anandamine (producing effects akin to cannabinoid-inducing euphoria) and interactions with several neurotransmitter systems (e.g. dopamine, serotonin and endorphins) as well as antioxidants including resveratrol, and other flavonoids; catechin, epicatechin, and procyanidins.[54],[55] However the authors suggest that the benefits are not sustained, with emotional “comfort” eating actually contributing to depressed mood.
Dark chocolate at doses between 6 – 40gms or so per day also confer cardiovascular benefits – via its polyphenolic compounds, immune benefits and stroke reduction – so keep it dark and in small daily doses.[56],[57],[58]
What To Avoid?
This list will seem depressingly familiar to all Nutritional Therapists as the nature of so many chronic illnesses involves activated and inappropriate immune promotion of inflammatory chemicals. The simple food suggestions listed here are to represent a starting point for supporting someone with a presenting complaint of mood or affect disorders.
I have contributed chapters to two books that along with the editor Martina Watts and colleagues explore the potential role of foods, food supplements and lifestyle change in the support of people with mental health issues.[59],[60] They provide far greater suggestions than can be delivered here.
A diet that contains saturated fats and refined simple carbohydrates and that lacks nutrient dense foods, vegetables and berries adversely impacts on our immune status, increasing inflammation, increasing oxidative stress and neurotrophins.[61] These are all understood to contribute to risk of depression.
First strike research published in 2011 confirmed that adolescent’s diet is linked to their mental health.[62] This also has implication in utero as compounded dietary related issues begin very early in life and, unless mitigated by advantageous food selection as affected individual’s age, the risk for mental health issues increases.
The perinatal environment plays an important role in programming many aspects of physiology and behaviour including metabolism, body weight set point, energy balance regulation and predisposition to mental health-related disorders such as anxiety, depression and attention deficit hyperactivity disorder, learning and behavioural disorders/autistic spectrum. Maternal health and nutritional status heavily influence the early environment and have a long-term impact on critical central pathways, including the serotonergic system and dopaminergic systems.[63] In other words we are never too young or old to benefit from lifestyle interventions as described in this article.
Conclusion
Healthier diets are associated with reduced mental health symptoms and unhealthy diets with increased mental health symptoms over time.[64]
Future Perspectives
Looking ahead the gut will almost certainly be a key area of focus for future studies. Not only is the gut the site of nutrient absorption, but also the resident microbial ecosystem of the gut may fine tune the threshold of inflammation and its impact on a wide range of chronic health conditions including those referred to as mental health.[65]
References
[1] Collins PY, Patel V, Joestl SS, March D, Insel TR, Daar AS; Scientific Advisory Board and the Executive Committee of the Grand Challenges on Global Mental Health, Anderson W, Dhansay MA, Phillips A, Shurin S, Walport M, Ewart W, Savill SJ, Bordin IA, Costello EJ, Durkin M, Fairburn C, Glass RI, Hall W, Huang Y, Hyman SE, Jamison K, Kaaya S, Kapur S, Kleinman A, Ogunniyi A, Otero-Ojeda A, Poo MM, Ravindranath V, Sahakian BJ, Saxena S, Singer PA, Stein DJ. Grand challenges in global mental health. Nature. 2011 Jul 6;475(7354):27-30. doi: 10.1038/475027a. View Full Paper
[2] Fournier, J. C., et al. (2010). Antidepressant drug effects and depression severity. JAMA, 303, 47-53. View Abstract
[3] Thomas LJ, Abel A, Ridgway N, Peters T, Kessler D, Hollinghurst S, Turner K, Garland A, Jerrom B, Morrison J, Williams C, Campbell J, Kuyken W, Lewis G, Wiles N. Cognitive behavioural therapy as an adjunct to pharmacotherapy for treatment resistant depression in primary care: the CoBalT randomised controlled trial protocol. Contemp Clin Trials. 2012 Mar;33(2):312-9. Epub 2011 Nov 11. View Abstract
[4] Herring MP, Puetz TW, O’Connor PJ, Dishman RK. Effect of exercise training on depressive symptoms among patients with a chronic illness: a systematic review and meta-analysis of randomized controlled trials. Arch Intern Med. 2012 Jan 23;172(2):101-11. View Abstract
[5] Scarmeas N, Luchsinger JA, Schupf N, Brickman AM, Cosentino S, Tang MX, Stern Y. Physical activity, diet, and risk of Alzheimer disease. JAMA. 2009 Aug 12;302(6):627-37. View Abstract
[6] Tangney CC, Kwasny MJ, Li H, Wilson RS, Evans DA, Morris MC. Adherence to a Mediterranean-type dietary pattern and cognitive decline in a community population. Am J Clin Nutr. 2011 Mar;93(3):601-7. Epub 2010 Dec 22. View Full Paper
[7] Ekmekcioglu C. Are proinflammatory cytokines involved in an increased risk for depression by unhealthy diets? Med Hypotheses. 2012 Feb;78(2):337-40. Epub 2011 Dec 6. View Abstract
[8] Crespi B, Summers K, Dorus S. Adaptive evolution of genes underlying schizophrenia. Proc Biol Sci. 2007 Nov 22;274(1627):2801-10. View Full Paper
[9] Raison CL, Miller AH. The evolutionary significance of depression in Pathogen Host Defense (PATHOS-D). Mol Psychiatry. 2012 Jan 31. doi: 10.1038/mp.2012.2. View Full Paper
[10] Handwerker WP. Cultural diversity, stress, and depression: working women in the Americas. J Women Health Gend Based Med 1999; 8: 1303–1311. View Abstract
[11] Dhabhar FS. Enhancing versus suppressive effects of stress on immune function: implications for immunoprotection and immunopathology. Neuroimmunomodulation 2009; 16: 300–317. View Full Paper
[12] O’Connor MF, Bower JE, Cho HJ, Creswell JD, Dimitrov S, Hamby ME et al. To assess, to control, to exclude: effects of biobehavioral factors on circulating inflammatory markers. Brain Behav Immun 2009; 23: 887–897. View Full Paper
[13] Kiecolt-Glaser JK. Stress, food, and inflammation: psychoneuroimmunology and nutrition at the cutting edge. Psychosom Med 2010; 72: 365–369. View Full Paper
[14] Giugliano D, Ceriello A, Esposito K. The effects of diet on inflammation: emphasis on the metabolic syndrome. J Am Coll Cardiol. 2006 Aug 15;48(4):677-85. Epub 2006 Jul 24. Review. View Abstract
[15] Calder PC, Albers R, Antoine JM, Blum S, Bourdet-Sicard R, Ferns GA, Folkerts G, Friedmann PS, Frost GS, Guarner F, Løvik M, Macfarlane S, Meyer PD, M’Rabet L, Serafini M, van Eden W, van Loo J, Vas Dias W, Vidry S, Winklhofer-Roob BM, Zhao J. Inflammatory disease processes and interactions with nutrition. Br J Nutr. 2009 May;101 Suppl 1:S1-45. Review. View Abstract
[16] Romier B, Schneider YJ, Larondelle Y, During A. Dietary polyphenols can modulate the intestinal inflammatory response. Nutr Rev. 2009 Jul;67(7):363-78. Review. View Abstract
[17] Sánchez-Villegas A, Delgado-Rodríguez M, Alonso A, Schlatter J, Lahortiga F, Serra Majem L, Martínez-González MA. Association of the Mediterranean dietary pattern with the incidence of depression: the Seguimiento Universidad de Navarra/University of Navarra follow-up (SUN) cohort. Arch Gen Psychiatry. 2009 Oct;66(10):1090-8. View Abstract
[18] Fung TT, Rexrode KM, Mantzoros CS, Manson JE, Willett WC, Hu FB. Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women. Circulation. 2009;119:1093-1100. View Full Paper
[19] Franco OH, Bonneux L, de Laet C, Peeters A, Steyerberg EW, Mackenbach JP. The Polymeal: a more natural, safer, and probably tastier (than the Polypill) strategy to reduce cardiovascular disease by more than 75%. BMJ. 2004 Dec 18;329(7480):1447-50. Review. View Full Paper
[20] Scarmeas N, Stern Y, Mayeux R, Manly JJ, Schupf N, Luchsinger JA. Mediterranean diet and mild cognitive impairment. Arch Neurol. 2009;66:216-225. View Full Paper
[21] Scarmeas N, Luchsinger JA, Schupf N, et al. Physical activity, diet, and risk of Alzheimer disease. JAMA. 2009;302:627-637. View Full Paper
[22] Singer SJ, Nicolson GL. The fluid mosaic model of the structure of cell membranes. Science. 1972 Feb 18;175(23):720-31. View Abstract
[23] Nicolson GL, Conklin KA. Reversing mitochondrial dysfunction, fatigue and the adverse effects of chemotherapy of metastatic disease by molecular replacement therapy. Clin Exp Metastasis. 2008;25(2):161-9. Epub 2007 Dec 5. Review. View Abstract
[24] Marazziti D, Baroni S, Picchetti M, Landi P, Silvestri S, Vatteroni E, Catena Dell’Osso M. Curr Med Chem. 2011;18(30):4715-21. Review. Mitochondrial alterations and neuropsychiatric disorders. View Abstract
[25] Agadjanyan M, Vasilevko V, Ghochikyan A, Berns P, Kesslak P, Settineri R, Nicolson G. Nutritional Supplement (NT Factor™) Restores Mitochondrial Function and Reduces Moderately Severe Fatigue in Aged Subjects. J Chronic Fatigue Syndr 2003; 11(3): 23-36 View Full Paper
[26] Sánchez-Villegas A, Verberne L, De Irala J, et al. Dietary fat intake and the risk of depression: the SUN project. PLoS One. 2011;6:e16268. View Full Paper
[27] Sánchez-Villegas A, Toledo E, de Irala J, Ruiz-Canela M, Pla-Vidal J, Martínez-González MA. Fast-food and commercial baked goods consumption and the risk of depression. Public Health Nutr. 2012;15:424-432. View Abstract
[28] Millichap JG, Yee MM. The diet factor in attention-deficit/hyperactivity disorder. Pediatrics. 2012 Feb;129(2):330-7. Epub 2012 Jan 9. View Abstract
[29] Cortés-Sánchez M, Morales-Muñiz A, Simón-Vallejo MD, Lozano-Francisco MC, Vera-Peláez JL, Finlayson C, Rodríguez-Vidal J, Delgado-Huertas A, Jiménez-Espejo FJ, Martínez-Ruiz F, Martínez-Aguirre MA, Pascual-Granged AJ, Bergadà-Zapata MM, Gibaja-Bao JF, Riquelme-Cantal JA, López-Sáez JA, Rodrigo-Gámiz M, Sakai S, Sugisaki S, Finlayson G, Fa DA, Bicho NF. Earliest known use of marine resources by Neanderthals. PLoS One. 2011;6(9):e24026. Epub 2011 Sep 14. View Full Paper
[30] Hedelin M, Löf M, Olsson M, Lewander T, Nilsson B, Hultman CM, Weiderpass E. Dietary intake of fish, omega-3, omega-6 polyunsaturated fatty acids and vitamin D and the prevalence of psychotic-like symptoms in a cohort of 33,000 women from the general population. BMC Psychiatry. 2010 May 26;10:38. View Full Paper
[31] Amminger GP, Schäfer MR, Papageorgiou K, Klier CM, Cotton SM, Harrigan SM, Mackinnon A, McGorry PD, Berger GE. Long-chain omega-3 fatty acids for indicated prevention of psychotic disorders: a randomized, placebo-controlled trial. Arch Gen Psychiatry. 2010 Feb;67(2):146-54. View Full Paper
[32] R.P. Heaney, “Nutrients, endpoints, and the problem of proof,” J Nutr, 138:1591-95, 2008. View Full Paper
[33] Ames BN. Prevention of mutation, cancer, and other age-associated diseases by optimizing micronutrient intake. J Nucleic Acids. 2010 Sep 22;2010. pii: 725071. View Full Paper
[34] Judge MP, Beck CT, Durham H, et al. Maternal docosahexaenoic acid (DHA, 22:6n-3) consumption during pregnancy decreases postpartum depression (PPD) symptomatology. FASEB J. 2011;25:349.7. View Abstract
[35] Berry extracts and brain aging: clearance of toxic protein accumulation in brain via induction of autophagy. Program and abstracts of the 240th National Meeting of the American Chemical Society; August 22-26, 2012; Boston, Massachusetts.
[36] Joseph JA, Shukitt-Hale B, Willis LM. Grape juice, berries, and walnuts affect brain aging and behavior. J Nutr. 2009 Sep;139(9):1813S-7S. Epub 2009 Jul 29. Review. View Full Paper
[37] Brewer GJ, Torricelli JR, Lindsey AL, Kunz EZ, Neuman A, Fisher DR, Joseph JA. Age-related toxicity of amyloid-beta associated with increased pERK and pCREB in primary hippocampal neurons: reversal by blueberry extract. J Nutr Biochem. 2010 Oct;21(10):991-8. Epub 2009 Dec 1. View Full Paper
[38] Goyarzu P, Malin DH, Lau FC, Taglialatela G, Moon WD, Jennings R, Moy E, Moy D, Lippold S, Shukitt-Hale B, Joseph JA. Blueberry supplemented diet: effects on object recognition memory and nuclear factor-kappa B levels in aged rats. Nutr Neurosci. 2004 Apr;7(2):75-83 View Abstract
[39] Krikorian R, Shidler MD, Nash TA, Kalt W, Vinqvist-Tymchuk MR, Shukitt-Hale B, Joseph JA. Blueberry Supplementation Improves Memory in Older Adults (dagger). J Agric Food Chem. 2010 Jan 4. View Full Paper
[40] Miller MG, Shukitt-Hale B. Berry Fruit Enhances Beneficial Signaling in the Brain. J Agric Food Chem. 2012 Feb 3. View Abstract
[41] Jacka F, Pasco JA, Mykletun A, et al. Association of Western and traditional diets with depression and anxiety in women. Am J Psychiatry. 2010;167:305-311. View Full Paper
[42] Pan A, Sun Q, Bernstein AM; et al. Red meat consumption and mortality: results from 2 prospective cohort studies [published online March 12, 2012]. Arch Intern Med. doi:10.1001/archinternmed.2011.2287. View Full Paper
[43] Wood JD, Enser M.Factors influencing fatty acids in meat and the role of antioxidants in improving meat quality. Br J Nutr. 1997 Jul;78 Suppl 1:S49-60. Review. View full Paper
[44] Wayerer S, Schäufele M, Wiese B, et al; German AgeCoDe Study group (German Study on Ageing, Cognition and Dementia in Primary Care Patients). Current alcohol consumption and its relationship to incident dementia: results from a 3-year follow-up study among primary care attenders aged 75 years and older. Age Ageing. 2011;40:456-463. View Abstract
[45] Peters R, Peters J, Warner J, Beckett N, Bulpitt C. Alcohol, dementia and cognitive decline in the elderly: a systematic review. Age Ageing. 2008;37:505-512. View Full Paper
[46] de Gaetano G, Di Castelnuovo A, Rotondo S, Iacoviello L, Donati MB. A meta-analysis of studies on wine and beer and cardiovascular disease. Pathophysiol Haemost Thromb. 2002;32:353-355. View Abstract
[47] Larsson SC, Orsini N. Coffee consumption and risk of stroke: a dose-response meta-analysis of prospective studies. Am J Epidemiol. 2011;174:993-1001. View Abstract
[48] Pasco JA, Nicholson GC, Williams LJ, et al. Association of high-sensitivity C-reactive protein with de novo major depression. Br J Psychiatry. 2010;197:372-377. View Full Paper
[49] Lucas M, Mirzaei F, Pan A, et al. Coffee, caffeine, and risk of depression among women. Arch Intern Med. 2011;171:1571-1578. View Abstract
[50] Juliano LM, Griffiths RR. A critical review of caffeine withdrawal: empirical validation of symptoms and signs, incidence, severity, and associated features. Psychopharmacology (Berl). 2004 Oct;176(1):1-29. Epub 2004 Sep 21. Review. View Abstract
[51] Patil H, Lavie CJ, O’Keefe JH. Cuppa joe: friend or foe? Effects of chronic coffee consumption on cardiovascular and brain health. Mo Med. 2011 Nov-Dec;108(6):431-8. View Abstract
[52] Rose N, Koperski S, Golomb BA. Mood food: chocolate and depressive symptoms in a cross-sectional analysis. Arch Intern Med. 2010 Apr 26;170(8):699-703. View Full Paper
[53] Parker G, Crawford J. Chocolate craving when depressed: a personality marker. Br J Psychiatry. 2007;191:351-352. View Full Paper
[54] Katz DL, Doughty K, Ali A. Cocoa and chocolate in human health and disease. Antioxid Redox Signal. 2011 Nov 15;15(10):2779-811. doi: 10.1089/ars.2010.3697. Epub 2011 Jun 13. Review. View Abstract
[55] Parker, G., Parker, I. & Brotchie, H. (2006a) Mood state effects of chocolate. Journal of Affective Disorders,92, 149– 159. View Abstract
[56] Buijsse B, Weikert C, Drogan, Bergmann M, Boeing H. Chocolate consumption in relation to blood pressure and risk of cardiovascular disease in German adults. Eur Heart J. 2010;31:1616-1623. View Abstract
[57] Larsson SC, Virtamo J, Wolk A. Chocolate consumption and risk of stroke in women. J Am Coll Cardiol. 2011;58:1828-1829. No Abstract Available
[58] Martin FP, Rezzi S, Peré-Trepat E, Kamlage B, Collino S, Leibold E, Kastler J, Rein D, Fay LB, Kochhar S. Metabolic effects of dark chocolate consumption on energy, gut microbiota, and stress-related metabolism in free-living subjects. J Proteome Res. 2009 Dec;8(12):5568-79. View Abstract
[59] Nutrition and Mental Health – a handbook. Edited by Martina Watts, published by Pavilion Publishing, 2008. Available Here
[60] Nutrition and Addiction: a handbook. Edited by Martina Watts, published by Pavilion Publishing, 2011. Available Here
[61] Jevtović S, Karlović D, Mihaljević-Peleš A, Šerić V, Vrkić N, Jakšić N. Serum Brain-derived neurotrophic factor (BDNF): the severity and symptomatic dimensions of depression. Psychiatr Danub. 2011 Dec;23(4):363-9. View Abstract
[62] Jacka FN, Kremer P, Berk M, et al. A prospective study of diet quality and mental health in adolescents. PLoS One. 2011;6:e24805. View Full Paper
[63] Sullivan EL, Smith MS, Grove KL. Perinatal exposure to high-fat diet programs energy balance, metabolism and behavior in adulthood. Neuroendocrinology. 2011;93(1):1-8. Epub 2010 Nov 13. View Full Paper
[64] Parrott MD, Greenwood CE. Dietary influences on cognitive function with aging: from high-fat diets to healthful eating. Ann N Y Acad Sci. 2007;1114:389-397. View Abstract
[65] Lawrence BP, Sherr DH. You AhR what you eat? Nat Immunol. 2012 Jan 19;13(2):117-9. doi: 10.1038/ni.2213. No abstract available.





